
Saving on Oxygen During Surgery at Kabwe General Hospital



Forty-eight-year-old Mulonda Kangili requires more oxygen than most. Though, he isn’t using it for (his own) breathing.
For the past 17 years, Mr. Mulonda has worked as an anesthetist/clinical officer at Kabwe General Hospital in Kabwe, Zambia. To deliver the type of anesthesia that puts patients “to sleep” and ensures they don’t feel pain during surgery (as opposed to local or regional anesthetics that numb only a particular area of the body), oxygen is required: as a patient breathes during surgery—either on their own or with the help of a ventilator—the anesthetic agent is turned into a vapor and is carried through into the bloodstream on the backs of oxygen molecules.
While oxygen might be all around us, the air we breathe only contains 21% oxygen; the purified, medical-grade form that anesthesia machines require to function is a lot harder to come by, particularly in low-resource settings like Kabwe. At Kabwe General, the staff can expect to go through approximately 30 oxygen cylinders per month. But when they run out of oxygen, they run out of the ability to provide safe anesthesia: the closest oxygen supplier is 90 miles (or 145 kilometers) away. For Mr. Mulonda, canceling surgeries due to oxygen shortages is just part of the job.
At least, it was.
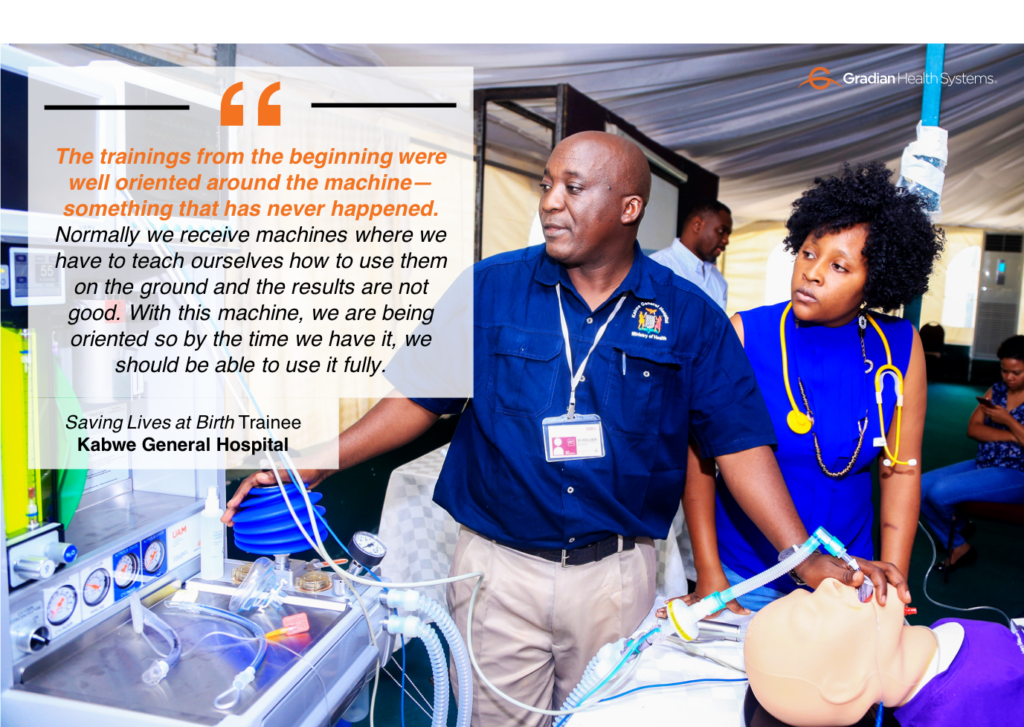
A few months ago, thanks to a grant from Saving Lives at Birth, Kabwe General received Gradian’s Universal Anaesthesia Machine (UAM). Because of the UAM’s built-in oxygen concentrator and ability to deliver anesthesia with room air, Kabwe now uses only 12 or 15 cylinders per month.
“Today, we no longer cancel patients. We are fine now,” says Mr. Mulonda.
“Today, we no longer cancel patients. We are fine now.”
Beyond the oxygen-saving benefits, the biggest difference between the UAM and anesthesia machines he’s used in the past is that his entire staff knows how to operate it. Mr. Mulonda told us that the UAM is the first anesthesia machine that included any sort of training. “Other equipment either you struggle reading the manual or maybe you come across a similar machine and find that you don’t fully utilize the equipment.”
To emphasize his point, Mr. Mulonda shared a story from the beginning of his career, when a brand new piece of equipment was donated to the hospital. “We tried to work with it, we lost I think two or so patients,” he explained, going on to say that other donated equipment has gone to waste because the practitioners were never adequately trained on how to use the machines.
Mr. Mulonda and the staff of Kabwe General aren’t the only ones who have been able to do their jobs more effectively since acquiring a UAM. After winning a grant from Saving Lives at Birth in 2017, we’ve equipped 9 other Zambian hospitals with the UAM, and we’re only a third of the way through our project. Check out our microsite to learn more.